A properly designed and validated sterilization packaging system ensures the effectiveness of the sterilization process and maintains sterile barrier integrity until it’s opened. This includes the full lifecycle of the packaging system—from raw material selection and material qualification, through forming, sealing, and sterilization, right through to distribution, warehousing, and final use.
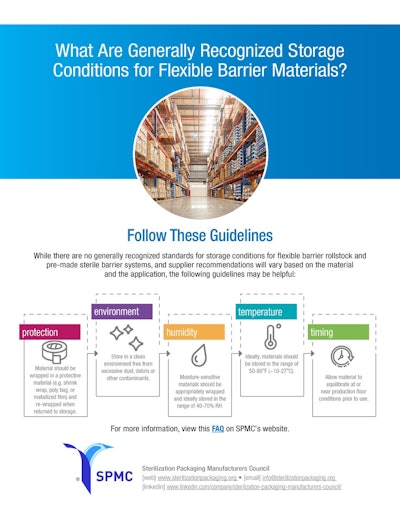
When it comes to the storage and handling of both rollstock packaging materials and preformed sterile barrier systems (pSBSs), packaging suppliers typically provide recommendations on temperature and relative humidity ranges, environmental conditions, protective wrapping, and a conditioning period prior to their use by a medical device manufacturer (MDM) or contract packaging facility. Following these recommendations helps optimize the quality of material being introduced into the production environment.
Sterility, however, is not solely the responsibility of the MDM. It’s equally critical for packaging manufacturers and device makers to ask the right questions early and often, proactively identifying potential risks and avoiding failures at every stage of the packaging journey.
To support this effort, the Flexible Packaging Association’s (FPA) Sterilization Packaging Manufacturers Council (SPMC) has released a free, three-part series of white papers that dive into the storage, transportation, and handling of sterile barrier systems. Two of the papers examine five key risk factors associated with the storage and handling of rollstock packaging materials and pSBSs. These include temperature, humidity, physical environment, protective measures, and time/equilibrium. A third paper provides an in-depth look at environmental conditions and specifically addresses the effects of cold temperatures (< 0 °C, including cryogenic conditions) on the storage and transport of sterile barrier systems.