Quality control is fundamental to manufacturing. Ensuring the consistency of inputs (supply chain, inventory, and components), processes and the production environment is essential to repeatability and efficiency.
Quality production is also critical for pharmacy automation devices, and not just the quality of automation systems themselves. As pharmacists increasingly automate various aspects of workflow, automation is turning the pharmacy itself into an environment where manufacturing concepts start to apply.
Regardless of whether a pharmacy is a large central fill facility serving a dozen provider sites or a small operation in a rural hospital, a pharmacy makes and delivers products while continually striving for quality, safety, and repeatable results.
However, when it comes to quality control in pharmacy manufacturing, there is perhaps no area more worthy of scrutiny than compounding, most of which continues to be done manually. There are two reasons such focus is important. First, compounding is one area where pharmacies actually process materials into products such as IV bags and syringes. But the more important reason is the risk of error or contamination in the manual compounding process. As the NECC situation demonstrated too clearly, such errors can result in patient injury, emergency intervention, extended hospitalization, or even death.
Because repeatability is a measure of quality control in manufacturing, manual compounding techniques have evolved to include several specific process steps performed in a cleanroom environment in order to reduce variability (i.e., error or contamination). And although studies of compounding technicians have found tremendous due diligence and a very low error rate, the biggest challenge to repeatability in manual compounding is simply that it is performed by humans. Despite their best efforts, people are fundamentally unable to achieve high repeatability, certainly not to the level automation can.
An analysis of manual compounding found the preparation of a single dose of Vancomycin can involve as many as 42 process steps, from writing and inputting the order, selecting the vial, measuring and mixing the compound, and delivering and administering it to the patient. At that rate, preparing only 24 doses would require more than 1,000 process steps.
But when you examine all the dose production steps involved, those most likely to be associated with patient injury occur in the pharmacy, and in particular during the compounding process itself (for example, selecting the wrong vial, calculating the wrong concentration, inadvertently contaminating the compound). Reducing the risk of variability in IV compounding is the purpose of automated compounding technology.
The goal of an ideal IV compounding automation system is to provide a solution that improves safety, efficiency, and productivity. Improving safety needs to address those areas where a fault analysis finds the potential for error. When considering an automated IV compounding system, examining the system’s quality controls and the extent to which they ensure repeatable results is one of the most important measures of system effectiveness. Toward that end, it is essential to consider these quality controls specifically:
• Environment and air flow. Under a laminar hood, a technician is supposed to hold the compound high in the airflow to ensure contact with first air. Likewise, in an automated compounding device, the compounding chamber should provide Class 5 laminar air, adequate airflow to clear the chamber ensuring particulate is swept away from critical areas, and provide continuous particle monitoring that will stop the process if contamination is detected.
• Product confirmation before use. This may seem fundamental, but errors occur here too frequently. In 2007, actor Dennis Quaid’s twin infants received adult doses of a blood thinner—1,000 times stronger than a pediatric dose—because a pharmacy technician drew medication from a vial with a label very similar to the vial that should have been used (both infants survived). An automated compounding system validates the inventory with barcode scanning to ensure the correct ingredient is used in every syringe or bag.
• Sanitization. Vial stoppers must be sanitized prior to fluid being drawn. The manual technique for effective sanitization requires several steps and includes wiping the stopper with alcohol and allowing the alcohol to evaporate—somewhat more rigorous than simply misting the vials with spray alcohol. Here again, the human element can result in variability of technique. An automated system should provide sanitization as well, and one of the most effective methods is pulsed UV light for vial stoppers and bag ports; automation further ensures proper positioning and exposure duration.
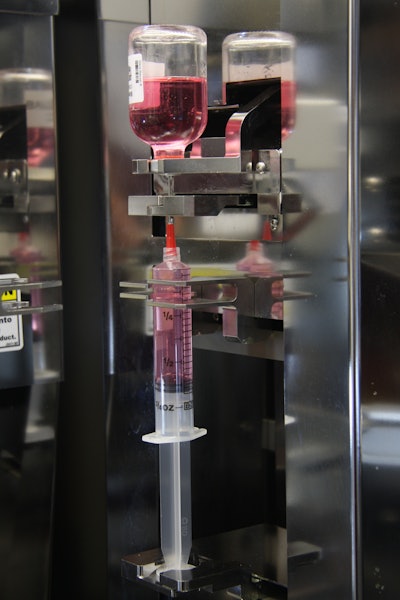
• Concentration. This is a particularly critical area because the wrong concentration can be fatal even if the right product is used. In manual compounding, technicians often use visual confirmation to determine when the right amount of fluid has been drawn into a syringe. Unfortunately, the line marks on a syringe barrel have only an approximate correlation to the actual interior volume, which can vary depending on brand and how they are manufactured.
In order to produce repeatable results, an automated system needs to be able to compensate for that variability. The best automated compounding systems do this by weighing the empty syringe, calculating the gravimetric weight of each fluid ingredient, and then weighing the syringe after each fluid is added to ensure the volume and concentration are correct.
• Pass-through systems. Just as in manual processing within clean rooms that use pass-through systems, automation should have loading and unloading methods that provide isolation from the background room and prevent outside air from entering the compounding areas.
• Output and administration. Ideally, a syringe or IV bag is labeled correctly with a barcode that matches a patient's wristband barcode. An automated compounding system should be able to do this too as one more measure of quality control.
Automated compounding technology is available and has produced millions of doses accurately. The most sophisticated systems already have features that can enhance compliance with USP<797>, as well as DQSA cGMP and tracking standards.
Pharmacies that are going to be best equipped to meet increased regulation in the future are those that have implemented automated pharmacy technology, especially automated compounding systems.
Regardless of how a pharmacy may see itself in the larger continuum of hospital services, the fact is a pharmacy’s dose production follows manufacturing processes and, just like in industry,quality control is essential. While pharmacies increasingly implement automated systems to enhance efficiency, automating IV compounding requires special consideration and thoughtful evaluation.
As products that are produced by a pharmacy, compounded IV medications are vulnerable to human error when produced manually—meaning that automated compounding technology must provide a solution for each step where the potential for error exists. An ideal automated IV compounding system will provide important quality controls to ensure repeatable results and medication safety.
Thomas Doherty is Executive Vice President, Technolog,y at ARxIUM (formerly Intelligent Hospital Systems). He has nearly three decades of experience developing medical devices, aerospace applications for aircraft, spacecraft and satellites, and naval command and control systems in a variety of platforms. He is co-inventor of 12 patents for technologies deployed in RIVA, a fully automated IV compounding system for pharmacies.