Ahead of this month’s, Pharmapack Europe 2024, Clare Beddoes and Stephen Augustyn from Cambridge Design Partnership discussed the latest on on-body large volume injectors (LVI) and what direction this product category is expected to take in 2024. They will be delivering a keynote address at the event during a dedicated track on Large Volume Drug Delivery on January 25th.
Q: What disease states do you feel are most untapped for on-body LVIs? What market changes have occurred in the past five years that led to this answer?
Clare: “It depends whether you look at the driver for on-body LVIs from the point of view of the disease or the requirements of the drug products in the pipeline that may best be served by those devices. On-body LVIs released to date have primarily addressed challenges associated with high-volume drugs – agnostic of disease - offering solutions for those formulations at volumes too high to be delivered via a single handheld device or have dosing regimens less applicable for infusion pumps. But if you look at the drug pipeline with a disease lens in terms of large volume drugs that could be appropriate for delivery via an on-body LVI, we see the often-mentioned conditions such as neurological disorders, oncology, and autoimmune diseases as presenting promising opportunities. Additionally, the current market trend towards less frequent dosing often requires higher drug concentrations in long-acting formulations which presents the challenge of higher viscosity. One approach to tackle this is dilution which increases the volume, thus creating another potential application for on-body LVIs. However, the advent of the 5ml AI devices has potential to erode the 2.25-5ml portion of the market previously applicable to on-body LVIs and at the other end of the volume range, >10ml may be better served by ambulatory infusion pumps.”
Stephen: “These systems are designed for fixed single doses and are well-suited for drugs with a wide therapeutic index if the patient will be tolerant to receive more than a minimum therapeutic dose. Market changes in the past five years, marked by the first approvals for devices in this category from West and more recently Enable, indicate a growing acceptance and adoption of on-body LVIs across various drug formulations.”
Q: Are there sustainability pros or cons compared to traditional autoinjectors/syringes that brand owners should be aware of?
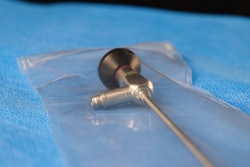
Stephen: “On-body LVIs are notably more complex than autoinjectors, involving adhesive patches, multiple sterility barriers, intricate fluid paths, and often electromechanical drive systems. Their sustainability is affected by factors such as selection of materials, potential introduction of electronics and batteries, manufacturing complexity, and larger transportation footprint. While there are some companies developing multiple-use devices, like the Gerresheimer Sensair and Nemera LVI, retaining the drive unit while replacing the drug container and fluid path introduces complexities for users.”
Clare: “One of the pros in terms of sustainability, can be derived from considering the alternative options for delivering the required volume, for example, for some of the large volume drugs like Repatha (evolocumab) and Skyrizi (Risankizumab), the dose delivered by a single on-body LVI would have to be delivered in two or more handheld devices (AI or prefilled syringe). Therefore, the life cycle analysis on such devices necessitates a comparison of the production and environmental impact of multiple handheld devices to one on-body delivery system. It’s not straight forward but I agree with Steve that the cons include materials, electronics, manufacturing complexity, and transportation burden. The pros may lie in enabling more patients to receive treatment at home, reducing travel and clinic resource usage. So, as you see the sustainability assessments are often complex and frequently multifaceted.”
Q: Would you say hurdles to commercializing and reaching patients are more cost-related, regulatory, or functional/material in nature?
Clare: “Two significant sources of inertia I would say are aversion to technical risk in the pharma industry and cost considerations. Companies are understandably cautious about risk and often prefer to launch in conventional devices initially. They're often not eager to add risk on top of risk with a new device for a new drug product. Technical complexities, novel primary containers that raise doubts over filling and product stability, device costs, and manufacturing for lower production volumes create hurdles. We’ve also seen that sometimes clinicians may not even be aware of on-body options due to cost-related formulary decisions, so accessibility and market education is crucial to overcome some of these hurdles.”
Stephen: “Regulatory challenges have seen a significant improvement since ISO 11608 Part 6 was published in 2022, offering a clearer framework. Unlike before, when these devices were verified as infusion pumps, which actually focus on ‘rate accuracy’ and not ‘dose accuracy’. So, I think the regulatory route is much better understood now and there are a couple of products on the market as well which gives some confidence to device manufacturers.
I also echo Clare's sentiments that technical and commercial challenges are stumbling blocks for on-body LVIs. The higher costs, especially for those that include electronics, pose many significant challenges. Pharma clients have told us of the cost scrutiny that these devices are subject to, and user preference alone may not be enough of an argument to justify one LVI over the use of two or more autoinjectors.
Whilst the regulatory framework is improving, approval bodies are still developing their understanding. At a London device conference I attended in January 2024, one major biologics company expressed frustration that some EU regulators see even the insertion of a drug cartridge for a single use device as evidence that the pump portion of the product is a standalone medical device. Such a device would require full compliance with the MDR including CE marking. Clearly, regulatory understanding is still evolving, so it’s important to talk to your regulator early and have a robust argument ready to defend your position.
From a patient's perspective, issues like adhesive patches and uncomfortable larger volumes and heavier devices can be barriers. Adhesives need to be strong enough to hold the weight of the device, but an overly aggressive adhesive can cause trauma to the skin during removal of the product. Whilst using an adhesive that’s too weak, or has not been properly applied by the patient, can lead to partial doses if movement causes a needle to disengage or a soft canula to occlude.
Also, the huge demand for high-volume biologics that was expected to drive on-body systems hasn't really materialized, or the devices are proving extremely complex and difficult to assemble. Even companies with substantial resources are struggling to resolve all the technical challenges and find a big enough market.
To summarise, the industry remains conservative, favouring established options like autoinjectors. Technical advancements, including gas and constant force spring drive systems, have addressed viscosity concerns. Some pharma companies have also told us that they are more comfortable using two autoinjectors (especially for loading doses) rather than deal with the complexity of an on body delivery system. As LVIs become more established, the anxiety around their use will diminish, but it’s taking a long time.”
Q: Have you observed—or do you expect—problems with automation (assembly/packaging), or do you feel solutions on the market are ready to handle the challenges?
Stephen: “Well, high-speed automation rarely makes sense below 2 million units a year. Below that volume, we're looking at semi-automated or manual processes due to the complex nature of the devices which adds a burden to the device cost. Some committed device manufacturers are pushing to enhance automation, but this does require very well considered device design and process monitoring.
The major snag we've encountered, and it's catching the attention of pharma clients, especially, is with non-standard primary containers. There's a real shortage of sterile fill-finish capability at the moment. Filling companies then face a decision – stick with what they know, like filling vials and cartridges, or take a risk with a complex novel primary container. These containers might not fit standard ISO bins for automated filling, or they might have a flexible component that introduces challenges in managing air bubbles throughout the process.
So, currently going for these novel containers doesn't seem like the most appealing option for fill-finish providers. Developing a filling strategy or choosing a container that will easily fit into current sterile fill processes is essential. On the other hand, products like the Enable LVI rely on the patient to handle the drug transfer, adding a layer of complexity. Even the Neulasta Onpro (a low volume on-body delivery system), requires the clinic to fill it at the point of use. Patient or HCP-filled devices may eliminate the sterile fill and stability issues, but they add a burden to the patient experience, which is going to factor in how likely they are to achieve a major commercial successes.”