Billions of medical devices are sterilized with ethylene oxide (EtO) each year. While EtO has made headlines and caused facility closures for unsafe environmental exposure and resulting health risks, for many years, there was no readily available process to serve as an alternative for medical device sterilization.
In 2019, the FDA set up innovation challenges to identify new sterilization methods and reduce EtO emissions. With limited facilities and significant device volumes, EtO sterilization providers become impacted leading to long lead times for sterilization.
At the[PACK]out this week, Megan Frost, PhD, and Kurt Yockey, both of Sterile State LLC, unveiled a new technology for medical device sterilization.
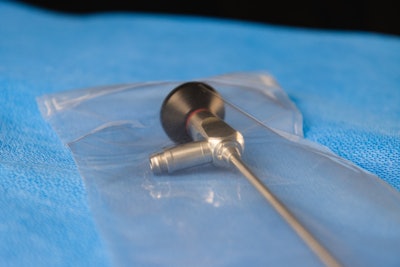
Yockey has worked with hospitals, nurses, medical device companies, and the Joint Commission is his tenure. “I'm here to introduce that our system is really very simple. Devices are placed into an enclosure, it's sealed, and then shipped immediately to customers. It's that simple,” he said. “There are no regional sterilization facilities, no sterilizer fees, no logistics, no delays, no waiting for sterilization, and it's completely safe.”
This technology, nitric oxide (NO) inside a polymer, was announced May 9. If successful, it could help assuage industry fears about having sufficient sterile medical devices while reducing risks to environments and worker safety.
Dr. Frost, CTO at Sterile State LLC, has worked on technology for 20 years, perfecting the sterilant and delivery system: “I started out using this technology to make implanted medical devices. The reason I'm telling you that is because it's a really safe technology, and it was developed to be at a standard much safer than what we used for packaging devices that aren't actually going to be implanted within the human body.”
The problem that Sterile State set out to solve is a large and multi-faceted one. 20 billion medical devices sold in the U.S. are sterilized with EtO, which is toxic at certain exposure levels. For years, the EPA and the FDA have asked the medical device industry to come up alternatives to EtO sterilization. Visit hcpgo.to/FDAeto
Nitric oxide and unique delivery
Beyond the unveiling of nitric oxide as a sterilant, Frost explained, “The second component to this innovation is the packaging. The way that we deliver the nitric oxide as a sterilant is through the packaging itself.”
![At the[PACK]out, Dr. Megan Frost discusses a breakthrough technology medical device sterilization: Nitric oxide.](https://img.healthcarepackaging.com/files/base/pmmi/all/image/2023/05/Dr._Megan_Frost_at_thePACKout.645c1d1b55cc2.png?auto=format%2Ccompress&fit=max&q=70&w=400) At the[PACK]out, Dr. Megan Frost discusses a breakthrough technology medical device sterilization: Nitric oxide.
At the[PACK]out, Dr. Megan Frost discusses a breakthrough technology medical device sterilization: Nitric oxide.
At its core, the technology works with nitric oxide embedded in a polymeric system—a polymer carries the molecule as a solid-state material that, under appropriate conditions, will release the nitric oxide. This means the nitric oxide is safely stored, and then safely released within the sterilization system after an activation period. “Because the carrier for our sterilant is a polymer, what we want to do is apply that sterilant to the packaging that we're going to use to encase medical devices,” she said.
- Activation: There are two activation modalities—room temperature or light. The light that is necessary is broadband white light.
- Compatibility: Initial development time has been spent on device compatibility. The process has been shown to be very gentle on electronics, epoxies, and more. Sterile State has not found polymers that are incompatible as of press time.
- Sterility and shelf-life: Sterility is maintained as long as the package barrier is maintained. As a relatively new application, the package itself has a one-year shelf-life prior to the device entering the system. That shelf-life study is ongoing.
- Polymers: Sterile State has developed approximately 27 different proprietary polymers that carry nitric oxide. These can be tooled to an MDM’s preference, and Frost noted that they are open to discussing an MDM’s specific applications and answering further questions.
With any new sterilization technology, it’s normal to question how an MDM can prove efficacy. As she explained, the sterilization efficacy of nitric oxide has been tested for log six reduction against all gram-positive and gram-negative E. coli, and spore formers. “When you look at the hierarchy of what the FDA requires to prove sterilization, the hardest species to kill are the spore formers. So that's used as the biological indicator to prove that we have actually reached sterilization. So we use the same biological indicator that's used with EtO: the spore former. When we put it in our system, we are able to eliminate it,” she said.
Related reading: Four Sustainability Updates in (and Around) Healthcare Packaging
During the presentation, Frost shared an image of paper strips in two petri dishes infused with bacteria. One dish was exposed to NO while the control was not. “Where you see the yellow halos means the bacteria is still growing after the four-hour exposure time. And the picture on the right-hand side where there is no halo indicates that the bacteria was completely eliminated…NO really is killing these infectious agents. We don't rely on a qualitative test to do this. We do quantitative microbiology, and if anybody has questions about this, I would be happy to go through how we do this. But we've proven quantitatively that we do reduce full log-6 reduction that's required,” she explained. ![As Kurt Yockey explained at the[PACK]out, a device is placed into an enclosure, it's sealed, and then shipped immediately to customers, precluding the need for regional sterilization facilities, sterilizer fees, and associated logistics, without risk of environmental harm posed by EtO.](https://img.healthcarepackaging.com/files/base/pmmi/all/image/2023/05/Kurt_Yockey_at_thePACKout.645c1d21d0d6c.png?auto=format%2Ccompress&fit=max&q=70&w=400) As Kurt Yockey explained at the[PACK]out, a device is placed into an enclosure, it's sealed, and then shipped immediately to customers, precluding the need for regional sterilization facilities, sterilizer fees, and associated logistics, without risk of environmental harm posed by EtO.
As Kurt Yockey explained at the[PACK]out, a device is placed into an enclosure, it's sealed, and then shipped immediately to customers, precluding the need for regional sterilization facilities, sterilizer fees, and associated logistics, without risk of environmental harm posed by EtO.
Frost also showed a chemiluminescence detection measurement, which is a measurement of nitric oxide within the packaging system. Upon activation there is a visible spike showing NO, which is sustained for the time at which it's exposed, and then it stops releasing.
Practical use
There are two main conditions that must be met for NO sterilization:
- As a gas sterilization technique, the device you want to sterilize must have gas contact (as it does with EtO). No box or chamber is needed—MDMs simply seal the package and sterilization will take place by sitting in the sealed packaging.
- The NO must be confined within the package, meaning that a gas impermeable membrane must encase the outermost layer of the package.
Frost explained that an MDM will purchase packaging materials from their packaging supplier. “The intention is that there will be no to very little change in machinery. We are using smarter materials with no change from the user's perspective,” she added.
NO could be placed in a number of spots in the package to cause sterilization to take place, including within a tray if there’s gas contact for the device, or an inner membrane in a double package system if the outer membrane is gas impermeable. “There's a lot of configurations we can use to take this polymer and make these device packages to allow us to sterilize these devices,” Frost said. “We can make soft packages that also enclose and encase the device we want sterilized, and it will become sterile. There are a lot of alternatives and options for how you can design the package to contain the NO release of polymer as long as we can find the polymer and allow gas contact with the device.”
EtO sterilization is confirmed via chemical and biological indicators. Sterile State has developed a chemical indicator that changes from a light color to a dark green. “So for my Michigan State friends, I always say to Kurt, this is your Spartan green indicator. As soon as it turns dark green, it's good to go. So green means go,” said Frost. “When the device has been sterilized, it reaches the appropriate dark green color, and you can see that sterilization has taken place. So the end result of this, here's the solution that we're proposing to answer the EtO challenge from the EPA and from the FDA, and that is you create a package that contains a polymer, you simply put your device in that package, you seal the package, and that device is ready to be shipped to a customer who wants to have that available for use.”
Safety and benefits
Frost pointed out that nitric oxide is safe for handling. “You are not required to use any special PPE when you're handling this. In fact, nitric oxide in its initial clinical application was for use in maturing neonatal lungs in babies. So it's safe enough that we can breathe it and be around it,” she said. “The sterilization takes place under ambient conditions, so you don't need special temperature or pressure to sterilize the equipment that you're using. There's no aeration as was needed with EtO. So the total sterilization time takes about four hours to complete as opposed to shipping it to an external source, sending it through the EtO system that takes 16 to 24 hours, and then returning it or shipping it to whoever's going to be using it.”
There are obvious environmental benefits to this—the sterilization cycle is shorter, there are no special environmental conditions needed, and the need to ship to and from a sterilization facility is eliminated. Frost noted that there are also no special chemical disposal requirements necessary.
During the Q&A, when asked why the technology hasn’t taken off yet, Frost noted, “The technology is new—we just developed it. This is the first time we've actually spoken about it publicly. The challenges with it are things like getting to the FDA, which we are before the FDA right now with an application on this. We’re working with a handful of medical device manufacturers who have different needs that we're looking at.”




![Speaking on sustainability at last year's the[PACK]out (from left): Lindsay Smaron, Samantha Smith, and Kevin Kane with Moderator Jamie Pero-Parker, PhD. Image: the[PACK]out](https://img.healthcarepackaging.com/files/base/pmmi/all/image/2023/04/sustainability_packout.6448509b2a6d2.png?auto=format%2Ccompress&fit=crop&h=167&q=70&w=250)