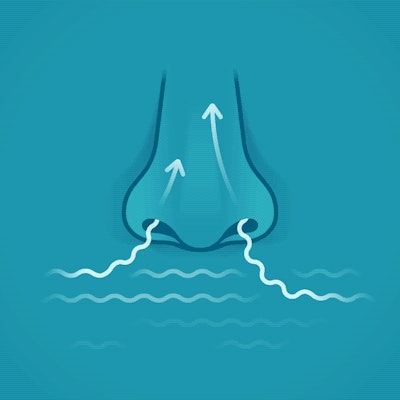
Nasal delivery of dry powder biologics offers promise in certain applications for efficacy, patient convenience, and logistics.
Because these stable powders don’t require temperature-controlled storage, their development can increase global availability to therapies and vaccines. There are also rare cases where injection is not an option for patients. For example, those suffering from Fibrodysplasia Ossificans Progressiva have a condition in which even minor injuries to muscle and connective tissue cause bone formation, leading to loss of mobility and serious health complications.
We delved into packaging considerations for nasal delivery devices in biologics, speaking to
Dr. Irene Rossi, Consultant Inhalation Technology, Pharma Services, Harro Höfliger, and Dr. Julie Suman, Vice President, Scientific Affairs, Aptar Pharma.
Current landscape and potential
Ahead of her talk at the AAPS National Biotechnology Conference in May, Rossi set the stage noting that one substance has already paved the way to approval: glucagon, a 29-amino acid peptide hormone. Available on the market as a nasal powder for systemic delivery, it’s used to treat very low blood sugar (severe hypoglycemia) in people with diabetes ages 4 years and above. It’s reportedly the number one prescribed glucagon in the U.S. A second substance, ONZETRA Xsail (sumatriptan nasal powder) is approved for treatment of migraines.
Both experts highlighted the potential of dry powder nasal delivery in vaccines, monoclonal antibodies, and even central nervous system (CNS) disorders. The delivery route offers advantages in comparison to nasal liquid formats for peptides and proteins because it can offer potentially longer residence time in the nose and may be formulated with bioavailability enhancers.
Notably in the case of vaccines, the potential elimination of cold chain requirements could boost vaccine accessibility worldwide, beyond centralized mass vaccination settings. Dry powder’s stability at room temperature facilitates global distribution, particularly benefiting developing countries and reducing logistical costs. Additionally, nasal delivery enhances patient-friendliness, enabling self-administration at home without specialized healthcare workers.
Related reading: Two Industry Leaders Working on Dry Powder Vaccine Delivery
Packaging components 101
These nasal sprays and powders are combination products where the formulation is delivered through a device (delivery system), which typically comprises (1) a vial or container, (2) a pump or actuator and aerosol generation system, and (3) a nosepiece, explains Rossi.
Because the final performance of the system is influenced by both the characteristics of the formulation and the device, the experts say it’s important to develop and assess the drug and device in parallel to speed time to market.
Devices can be active or passive. An active device operates independently of the patient’s inhalation or blowing, using a pressure chamber or a propellant to disperse the dry powder. “Passive nasal devices require the user to generate an airflow by blowing or sniffing into the device in order to deliver the dry powder into the nose,” says Rossi. Each type has pros and cons, so it’s wise to assess which route fits an application earlier on.
She adds that a target patient population such as children may have difficulties in coordinating their breath to blow correctly into the device, or elderly patients may not have enough strength to actuate the pressure chamber. She adds that active delivery systems usually offer a better and reproducible deagglomeration mechanism (essentially, the breakdown of clumps without impact to the particles themselves), which depends less on the patient population.
With an injection, a patient can typically see when the dose is delivered, or feel when the plunger has depressed all the way. But how does this work with nasal delivery?  Aptar Unidose Powder system.
Aptar Unidose Powder system.
It may be easier to tell that a dose has been delivered correctly with active delivery. In the case of Aptar’s Unidose Powder system, the active device generates the aerosol. There’s a certain minimum force to actuate, which is achievable by a range of patients. “In the case of glucagon nasal powder, which is already on the market, the instructions for use are not to inhale with the powder, so there is no coordination [with breath and administration]. With our Unidose Powder, you don't have to coordinate an inhalation with the device which takes away some of that user variability,” says Suman.
Of course, there could still be some insertion variability or range of motion in the nose, so clear instructions for use or even training kits come into play, Suman adds. Aptar’s sister company, Noble, helps companies with development of instructions for use and training devices.
Secondary packaging must offer robust protection to prevent moisture ingress and offer long term stability for biomolecules. Rossi says moisture uptake can change the powder’s physical properties—and therefore deposition in the nasal cavity—and degradation. Here, active films and blisters can play a role in moisture protection.
Formulation and stability
When re-formulating from traditional liquid formulations to nasal powders, companies employ long-established techniques such as lyophilization and spray drying.
In general, Suman says Unidose Powder system contain anywhere from 10 to 80 milligrams of product, including excipients, depending on the density of the powder. For those looking to transition from a lyophilized, injectable powder to a nasal or inhalation powder, she notes that a freeze-dried material typically requires some form of additional post-processing, either mixing with another carrier or mixing to optimize the powder to be aerosolized. “The lyo cake itself is not necessarily suited for dosing and aerosolization. For those that are on the injectable side, there's usually another step before you can fill into the device,” she adds. Lyo cake properties make it difficult to dose at a high mass, especially due to low density.
Rossi explains that particle engineering combined with selecting the right excipients (inactive components) benefits the manufacturing process, as it allows control over powder properties, such as particle size, water content, and solid state. These properties are key to maximizing product deposition in the nasal cavity—which will prevent the drug from entering the lungs—and controlling powder dissolution and thus bioavailability, she says. “Handling of these particle engineered powders can be particularly challenging due to their micron-size, moisture uptake and, for some biologics, also degradation due to oxidation, reduction, aggregation. Hence, specific filling technologies have been developed and are available to load these powders into the primary container (i.e. vial, reservoir, capsule, etc.), being employed already at early development bench top equipment that is easily scaled up to commercial production, such as Harro Höfliger Drum Lab.”  Harro Höfliger Drum Lab.
Harro Höfliger Drum Lab.
Single- vs multi-use
Currently, commercialized applications for nasal dry powder medications are all single-dose due to their therapeutic application: Unidose Powder, a single-use plastic cartridge delivery system, and Optinose, a capsule device.
“The capsule device consists of a reusable body used to load, pierce, and deliver the dry powder contained in the capsule, so it can be considered a multi-use device. While Optinose's capsule device technically allows for multiple uses, it's primarily a single-dose system. However, there's ongoing exploration of multi-dose solutions, including reservoir-based or pre-metered devices,” says Rossi.
Though not yet available commercially, concepts like reloadable nosepieces are being explored to address contamination concerns for multi-dose systems. When developing a multi-use device, it’s important to study long-term stability and protection of powder from physical, chemical, and structural degradation.
Suman highlights growing interest in multi-dose nasal powder formats particularly for monoclonal antibodies in the infectious disease arena for prophylaxis or infection treatment, where extended treatment durations of seven to 14 days would necessitate multi-dose systems. She says there’s also a small subset of companies looking at powder delivery for chronic administration.
The advantages of nasal powder delivery, such as avoiding cold chain storage and delivering higher payloads, have fueled interest for biologics. The challenge lies in balancing sustainability with reloadability to minimize plastic waste.
Current challenges
Of course, there are always complexities when entering new device territory for biologics. These molecules are often fragile, requiring meticulous handling to prevent damage and maintain their efficacy. Working with molecules in the early stages of development adds uncertainty to the process.
There are also technical challenges associated with device functionality and cost. Unlike traditional vials and syringes, nasal delivery devices are more complex and costly to develop due to the need for active powder dispersion mechanisms. This complexity extends to the combination of the device with the formulation, requiring careful evaluation of factors like dose reproducibility, particle size distribution, and material selection. Human factors such as usability and patient handling must also be studied early.
The regulatory landscape presents challenges for any new device, but specific guidelines and testing protocols are emerging for nasal powders. Rossi highlights that the USP chapter for testing of nasal powders was recently reviewed, resulting in “a differentiation when assessing the drug in small particles for nasal powders versus nasal sprays.”
Despite the obstacles, two dry powder nasal products have made it to market, and other companies are developing devices (currently in concept/prototype phase) which are designed to be used off-the shelf for new dry powders.
Sustainability benefits and trade-offs
As is mentioned above, the elimination of cold chain requirements reduces environmental impact compared to traditional delivery systems. However, the production of nasal delivery devices may involve more materials due to their complex components and the need for robust secondary packaging for stability. Device companies are exploring recyclable materials and renewable feedstocks, as well as reusable devices to reduce the environmental footprint of single-use systems for certain applications.
Of course, cost of goods is an important consideration, particularly in the vaccination space where there are already well-established injectables, says Suman. “Here, a nasal powder that has fewer injection molded parts comes into play.”
Aptar is developing a blister for these situations. Powder is filled into a blister, which is then inserted into a device with a reduced number of parts, the user closes the flap, piercing the blister, and then they inhale.
Is automation ready?
As development is underway, pharmaceutical manufacturers may have concerns about the maturity of assembly and packaging lines for novel devices. Experts say automation for both assembly and packaging of dry powder nasal delivery devices is increasingly ready for industrial-scale production.
Primary and secondary packaging solutions are already established and validated for commercialized nasal powder products, says Rossi, adding that drum dosing systems precisely fill dry powder into containers. Assembly and labeling processes have been developed for both low-speed (approximately 25 to 30 ppm) and high-speed solutions (up to 200 ppm), or are under development for late-stage clinical trials.
However, challenges may arise due to powder characteristics (including micron-size and density) which may make it difficult to implement standardized solutions directly.
Rossi reiterates that companies should consider packaging solutions early during development to ensure compatibility with available systems. Co-development of formulation, device, and processing pathways will expedite the transition to clinical trials and commercialization.
The question, says Suman, is whether a drug needs to be preservative-free on the aqueous side. “For powders, this isn’t an issue because you can perform microbial testing of the powder itself. But if someone had a special request in terms of the relative level of the cleanroom for manufacturing, then that might become one point of concern. But the Unidose Powder is industrialized, it's filled [employing Harro Höfliger powder technology] by a number of different contract development and manufacturing organizations (CDMOs).”
For early-stage customers that aren’t quite ready for commercial material, Aptar and Harro Höfliger both produce kits to help companies fill at the bench scale.
Next steps and other points to consider
Experts agree that it’s important to test and evaluate primary packaging solutions at an early stage, particularly because it can impact final product performance (especially for passive devices). Overall, more awareness of dry powder nasal delivery is needed in the biologics space. But Suman says she is seeing a trend in customers approaching earlier in their process than before—in the preclinical phase—exploring the best route to deliver the drug.
Aptar fields requests regarding how they can support preclinical studies. For non-human primates, the nasal devices typically fit into the nose cavity. “For smaller animals‚ you need to taper down the outer diameter of the actuator. We have means to accomplish that, either by using a pediatric device or adding a sleeve to taper the device. We've also developed two devices that can be used for mice and rats,” Suman says.






![Alison Bryant, senior consultant at Antea Group and communications director for the Healthcare Plastics Recycling Council (HPRC), addressed the crowd at the[PACK]out.](https://img.healthcarepackaging.com/files/base/pmmi/all/image/2024/05/Alison_Bryant.6644005a513b0.png?auto=format%2Ccompress&fit=crop&h=167&q=70&w=250)