Major market regulators and international standards bodies have upped the ante for control of the end-to-end pharmaceutical supply chain, starting with the ingredients.
In 2015, the EU Commission published Good Distribution Practices for Active Pharmaceutical Ingredients, not just Good Manufacturing Practices.
Mark Paxton, CEO of Rx360, the international consortium for safe supply of medicines, says, “Concern has been growing across all regulatory authorities in all regions about the ability to ensure the quality of drugs and their components as they move in international commerce. Thus, collaboration (between regulatory agencies) has increased out of necessity. Implementation of the EU’s Falsified Medicines Directive in 2012 serves as a catalyst for much of this collaboration.”
The U.S. Drug Supply Chain Security Act (DSCSA) of 2013 is the other major overarching guidance.
Regulatory expectations
Any company procuring, importing, supplying, manufacturing or exporting active substances is required to follow the new EU GDP for APIs guidelines, whose core principles include the following:
• You need a QMS—“2.1. Distributors of active substances should develop and maintain a quality system setting out responsibilities, processes and risk management principles.” The QMS should include deviations from SOPs are documented; CAPAs undertaken to correct and prevent deviations; and changes that may affect storage and distribution of active substances are evaluated.
• You need Quality Agreements—“6.12. Where storage or transportation of active substances is contracted out, the distributor should ensure that the contract acceptor knows and follows the appropriate storage and transport conditions.”
• One QP responsible—“3.1. The distributor should designate a person at each location… that should be trained on the requirements of GDP for active substances.”
• Effective temperature monitoring—“5.1. Monitoring devices that are necessary to guarantee the quality attributes of active substances should be calibrated according to an approved schedule against certified traceable standards.”
• Prove temperature control in your facilities—“6.4. Active substances subject to specific storage measures, e.g. narcotics and products requiring a specific storage temperature or humidity, should be immediately identified and stored in accordance with written instructions and with relevant legislative provisions.”
Dear API supplier: Where is your QMS?
Today’s APIs have strict temperature monitoring, analytic testing and quality control requirements. Most shipments contain little QC information accompanying the delivery of drug substances to the pharmaceutical company.
However, when a massive bulk quantity of a common API can be used for up to five years manufactured into final dosage, how can the pharmaceutical industry or company guarantee its shelf life? Pharma wants API suppliers to perform long-term stability studies for their products, and provide more clear temperature requirements stated on the label of each bulk shipment of APIs.
The EC 2014 update to GMP for API says, “The (API) manufacturer shall issue certificates of analysis for each batch of active substance upon the request of competent authorities, distributors and/or manufacturers of medicinal products supplied directly or indirectly with the active substance.”
So the question is, “Why doesn’t this QC information make it to the shipping label or purchasing documents?”
Temperature control requirements
One of the biggest challenges with APIs is the lack of any stability data, which requires tighter temperature control until the stability limits are understood. In the pack-out process, temperatures can vary considerably for very low temp applications, dry ice or liquid nitrogen dioxide, or LN2.
Managing these different temperature control requirements is complex. The pharmaceutical industry needs shipping systems and data loggers that can handle all temperature extremes for an entire API supply chain, ideally into final dosage manufacturing to ensure the same types of data sources and ability to statistically compare the data over time.
Stability budget – the solution for a drug’s lifecycle?
A stability budget is a methodology that assigns each leg of a product lifecycle or supply chain a certain amount of stability data. So instead of shipping strict 2°C to 8°C temperature range, with no variables or allowances, you allow each leg of the supply chain some lenience to use a small part of a stability budget—thus reducing temperature alarms, QA investigations and wasted resources.
Some pharma companies manually allocate stability along the lifecycle, whereas future methodologies include “pushing stability budget forward.” This becomes possible with modern IT systems such as central databases for temperature monitoring data that would track the information.
However, drug substances and APIs have little stability data available. Therefore they wouldn’t be factored into a stability budget. But when do drug substances become a finished product? Is there a gray area when stability of a “product” starts and stops? Monitoring and using stability data during the entire cold chain of a product "from API to end user" is used more frequently.
So-called “warm times” occur during the fill-finish process. According to the FDA Drug Security Act and EU GMP Annex 15—any and all GMP environments must be quality controlled, which most often means temperature monitoring of cleanrooms and biological processing rooms.
Bottom line—who’s connecting the dots through the lifecycle of a product to ensure patients downstream that their medicine is safe to be consumed?
Dear pharmaceutical manufacturer: What controls do you have in place?
Who’s responsible for ensuring your APIs are quality controlled from inception? Is that the responsibility of your 3PL or specialty courier handling temperature-controlled vats of biological APIs? How involved in the process do you get as a pharmaceutical manufacturer beyond basic GMP qualification of API vendors?
Beyond the mandatory Quality Agreements, what else can pharma do to ensure quality control of their drug substances?
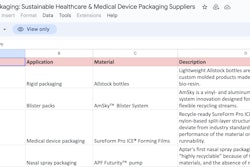
• Choose the right supply chain partner and shipping solution. However, some pharma practitioners say there are not many options for bulk shipping systems.
• Ask your courier or 3PL if they perform lane qualifications, and if they have they qualified lanes that you will be using?
• Ship by sea for low-value API. But caution, the reefer needs to be full to ensure complete circulation and effective temperature control.
• Can API suppliers send smaller quantities? Why not sell at bulk prices, and offer pharma fees to hold stock and ship as needed? Is a “consumption model” a future scenario?
Conclusion
API manufacturers must bring their facilities, methods, processes, systems and controls into compliance with GDP and GMP standards or pharmaceutical manufacturers won’t do business with them.
For pharma manufacturers, regulators are looking for evidence that companies are mapping their entire supply chains from ingredients through R&D and into manufacturing supply chains. Every step in the drug’s lifecycle must be quality controlled, monitored and documented—from inception to consumption.
Editor's note: Courtney Becker-James is the Strategic Marketing Director for Elpro, a provider for the monitoring of environmental conditions throughout the supply chain of perishable goods.